Urology Case Reports
Prostate tumor metastasis in cecal appendix diagnosed after appendicitis in a virgin treatment patient: A case report
Author links open overlay panelTadeu JFL.CamposLucas De O.LimaFrancisco E DeV FilhoAndré CM.LimaAna CM DeQueirozMarcos FH.Rocha
- Hospital Geral de Fortaleza, Brazil
Received 1 November 2020, Revised 30 November 2020, Accepted 1 December 2020, Available online 4 December 2020, Version of Record 8 December 2020.
Abstract
Involvement of cecal appendix by metastases secondary to prostate cancer is extremely rare. We have reported a case of a patient with an acute abdomen who underwent right hemicolectomy for appendicitis. Immunohistochemistry of the appendix revealed a prostate tumor metastasis. The presence of prostate cancer metastasis in the cecal appendix is rare, with less than 10 cases reported in published literature. Involvement of the cecal appendix secondary to prostate cancer must be considered as a differential diagnosis in cases of appendicitis, especially in patients who already have a diagnosis of metastatic prostate cancer.
Keywords
Introduction
With the advent of the PSA marker and the implementation of prostate cancer screening programs, its epidemiological scenario has dramatically changed in recent decades. Early diagnosis of prostate cancer has started to become the trend, with a large number of diagnosed yet asymptomatic patients and with localized tumors.1
Despite the spread of screening programs and recommendations made by major urological societies, many patients do not regularly undergo screening for prostate cancer. Due to this, although in a much smaller number, we still find patients diagnosed with prostate cancer in advanced stages; some patients also have disseminated metastases, which are incurable. Prostate cancer has a great predilection for bone metastases, with visceral metastases being present in more advanced or atypical cases. Among the visceral metastases in prostate cancer, the most common sites are the lungs, liver, and adrenal gland.2
Acute appendicitis is the main cause of acute abdomen, and is an important and frequented cause of emergency surgery. Appendicolith and lymphoid hyperplasia are the most relevant causes in the etiology of appendicitis. Appendicitis can also, albeit rarely, be induced by metastatic disease in the lumen.3
In this article, we present a case of metastatic prostate cancer diagnosed by immunohistochemical analysis of the cecal appendix of a right hemicolectomy surgical specimen performed in an emergency due to acute abdomen.
Case report
A 64-year-old male black patient was admitted to the emergency department of Hospital Geral de Fortaleza on December 27, 2019. On admission, he complained of abdominal pain he had been experiencing for one month that intensified within the last ten days. He also noted and reported that his abdominal pain was also associated with significant weight loss.
The patient denied comorbidities and medications of continuous use. He had not previously undergone surgical approaches. Denied relevant family history of prostate cancer. He reported being a former smoker.
On examination, he was in regular general condition, with a distended abdomen, tympanic on percussion, painful on palpation, and exhibiting signs of peritonitis. Abdominal radiography was performed to identify pneumoperitoneum, and emergency surgery was indicated after vigorous hydration and initiation of antibiotic therapy.
Exploratory laparotomy was done on the same day of admission. During surgery, probable carcinomatous masses in the mesentery were identified. In addition to gas dissecting the omentum, there was also an important inflammatory block in the hepatic flexure region of the colon, cecum, and appendix.
Due to intraoperative findings, the patient underwent a right ileocolectomy with terminal ileostomy. The surgery was performed by an experienced general surgeon. On the seventh day after surgery, the patient presented with an infection of the surgical wound, which progressed further after three days. He then underwent a second surgical procedure for abdominal wall resection, and progressed satisfactorily after surgery; he was discharged on the thirteenth day after admission.
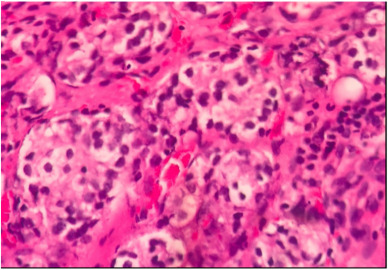
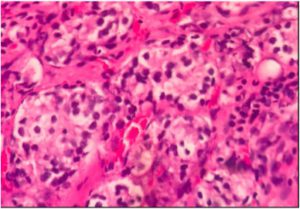
The anatomopathological examination of the right ileocolectomy specimen showed atypical acinar proliferation in the subserosa of the cecal appendix. The immunohistochemical evaluation results were positive for anti-PSA and negative for anti-CD56, anti-CDX2, and anti-chromogranin A, concluding that it was an adenocarcinoma of the primary prostatic immunophenotype infiltrating the serous appendix (Fig. 1).
 Fig. 1. Computed tomography showing prostate without cleavage plan with Bladder and rectum, in addition to lymph node enlargement.
Fig. 1. Computed tomography showing prostate without cleavage plan with Bladder and rectum, in addition to lymph node enlargement.The serum dosage of PSA in April 2020 was 42.67 ng/dL. On rectal examination, a prostate weighing approximately 60 g with a stone-like, fixed aspect was identified. This suggests that it is a locally advanced prostate tumor, with a T4 clinical stage.
In june 2020, 2 patient underwent a random transrectal biopsy of the prostate. From this, eight specimens were acquired. On anatomopathological analysis, all the fragments revealed that it was Gleason 3 + 4 acinar prostate adenocarcinoma.
For staging, a contrast computed tomography (CT) of the abdomen and pelvis was performed. In this examination, a volumetric enlargement of the prostate was identified, which presents itself with undefined contours without a cleavage plane in the posterior wall of the bladder and anterior wall of the rectum. Lymph node enlargement was also observed in the iliac and interaortocaval chains (Fig. 2). To complement the staging, bone scintigraphy was performed, which showed areas of secondary involvement in the skull, spine, rib cage, pelvis, and femurs.

Fig. 2. Atypical acinar proliferation in subserosa of the cecal appendix.
Discussion
In our country, it is not uncommon to diagnose prostate cancer in advanced stages, either by local tumor complications or by symptoms of metastatic disease.
Advanced prostate cancer, when metastatic, has a great predilection for bone involvement in the form of osteoblastic lesions. The most commonly affected sites are the spine and the bony pelvis.2
Non-bone or visceral metastases are uncommon and generally denote a more advanced disease with an unfavorable prognosis, classifying the patient as high-volume metastatic according to the CHARTEED criteria.4
In general, only 0.9% of acute appendicitis cases are caused by neoplasia. Of these cases, less than 15% are caused by metastasis. Metastasis of prostate cancer in the cecal appendix is extremely rare, having less than ten cases being reported.5
We reported a rare case, in which the initial diagnosis of prostate cancer was made based on immunohistochemical analysis of the cecal appendix of a right ileocolectomy surgical specimen performed in an emergency acute abdomen patient without a previous diagnosis of cancer. The immunohistochemical evaluation was positive for anti-PSA and negative for anti-CD56, anti-CDX2, and anti-chromogranin A.
Our case was unique because the patient was diagnosed with prostate cancer secondary to an episode of acute appendicitis that required emergency hemicolectomy.
Conclusion
Despite the popularization of prostate cancer screening programs, we are still faced with late-stage diagnoses, such as what is seen in this case; the patient in question, in addition to local tumor extension and multiple bone metastases, also had visceral metastasis in the cecal appendix.
The involvement of the cecal appendix secondary to prostate cancer is extremely rare; however, it must be considered as a differential diagnosis in cases of appendicitis, especially in patients who already have a diagnosis of metastatic prostate cancer.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
The ethical approval was provided.
Consent
Informed consent had been obtained from the patient.
Author contribution
Tadeu José Fontenele Leite Campos: study concept, data collection, data interpretation, and writing the paper.
Marcos Flávio Holanda Rocha: data collection, data interpretation and writing the paper.
Francisco Eugênio de Vasconcelos Filho: data collection and writing the paper.
Lucas de Oliveira Lima: data collection and writing the paper.
Ana Carolina Matos de Queiroz: data collection.
André Costa Matos Lima: data collection.
Registration of research studies
Not Applicable (Case Report; not an interventional study).
Guarantor
Tadeu José Fontenele Leite Campos.
Declaration of competing interest
This manuscript has no conflicts of interest to disclose.
Acknowledgement
Authors would like to give their biggest gratitude to the Department of Urology and Oncology of Hospital Geral de Fortaleza.
References
- 1
-
R. Etzioni, J.M. Legler, E.J. Feuer, R.M. Merrill, K.A. Cronin, B.F. Hankey
Cancer surveillance series: interpreting trends in prostate cancer—part III: quantifying the link between population prostate-specific antigen testing and recent declines in prostate cancer mortalityJ Natl Cancer Inst, 91 (1999), pp. 1033-1039 - 2
-
L. Bubendorf, A. Schöpfer, U. Wagner, et al.
Metastatic patterns of prostate cancer: an autopsy study of 1,589 patientsHum Pathol, 31 (2000), pp. 578-583 - 3
-
B.A. Birnbaum, S.R. Wilson
Appendicitis at the millenniumRadiology, 215 (2000), pp. 337-348 - 4
-
C.E. Kyriakopoulos, Y.H. Chen, M.A. Carducci, et al.
Chemohormonal therapy in metastatic hormone-sensitive prostate cancer: long-term survival analysis of the randomized phase III E3805 CHAARTED trialJ Clin Oncol, 36 (2018), p. 1080 - 5
-
S.J. Connor, G.B. Hanna, F.A. Frizelle
Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7970 appendectomiesDis Colon Rectum, 41 (1998), pp. 75-80